Pediatric Otolaryngology
(365) Parental Perception of Nighttime Breathing in Children with down Syndrome
Monday, October 2, 2023
2:45 PM - 3:45 PM East Coast USA Time
Has Audio

Carolyn A. Chabuz, MD
Resident physician
University of Colorado SOM
Denver, CO, United States
Carolyn A. Chabuz, MD
Resident physician
University of Colorado SOM
Denver, CO, United States
Presenting Author(s)
Co-Author(s)
Disclosure(s):
Carolyn A. Chabuz, MD: No relevant relationships to disclose.
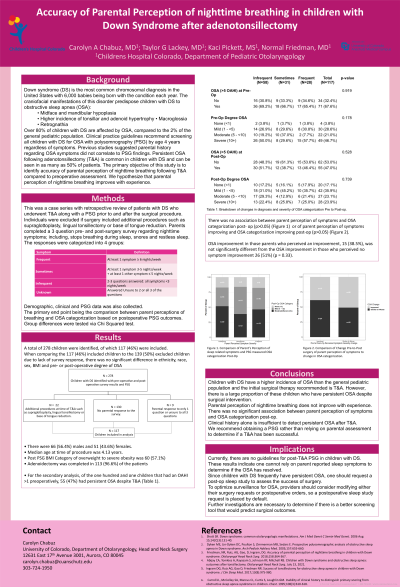
Introduction: Clinical practice guidelines recommend screening all children with Down syndrome (DS) for obstructive sleep apnea (OSA) with polysomnography (PSG) by age 4 years, regardless of symptoms. Previous studies suggested parental history regarding OSA symptoms did not correlate to PSG findings. Since persistent OSA (OAHI > 1) following adenotonsillectomy (T&A) is common in children with DS, it is important to know if clinicians can rely on parental assessment postoperatively. The primary objective of this study is to identify accuracy of parental perception of nighttime breathing following T&A compared to preoperative assessment.
Methods: Case series with retrospective review at a tertiary care academic pediatric hospital.: Patients with DS who underwent T&A along with a PSG prior to and after the surgical procedure were included. Parents completed a 3 question pre- and post-surgery survey regarding nighttime symptoms. The responses were categorized into 3 groups: infrequent < 3 nights/week on all questions answered, sometimes where they have >3 nights/week but < 6 nights/week, or frequent 6 or greater nights/week on at least 1 question. The primary end point being identifying the accuracy of parental perception of nighttime breathing in children with DS following T&A.
Results: A total of 256 children met inclusion criteria, of which 117 (46%) were included. A total of 71 (68%) children had an obstructive apnea hypopnea index (OAHI) >5 preoperatively compared to 55 (47%) post-operatively. There was no association between parent perception of symptoms and OSA categorization post-op (p>0.05) or of parent perception of symptoms improving and OSA categorization improving post-op (p>0.05). Parents were unable to predict OSA status despite having previously encountered symptoms of OSA (p = 0.758)
Conclusions: Despite previous experience, parents are unable to predict nighttime breathing patterns following a T&A. We recommend obtaining a PSG rather than relying on parental assessment to determine if a T&A has been successful.
